Out of all babies born in 2015, 83.2% were breastfed. Breastfeeding can be some of the most joyous moments you share with your new baby. It allows you to form a deeper connection with your child while providing them with the vital nutrients they need to survive, grow, and stay healthy.
But, breastfeeding can also be nerve-racking for first-time moms. Whether you’re not sure how to breastfeed effectively or you’re trying to decide between breastfeeding and formula-feeding, don’t worry. We’re here to help. We’ve gathered everything you need to know to make a decision about breastfeeding as well as information and tips to help make breastfeeding more successful once you begin.
It’s important to remember that deciding to breastfeed is a personal choice and how you raise your baby ultimately comes down to your preference. Also, remember that breastfeeding is a learned skill — a journey that you and your baby will embark on together as you welcome the newest addition to your family.
What You Can Do Before Your Baby is Born
Before your baby is even born there are a few things you can do to prepare and make your breastfeeding experience go more smoothly once your baby arrives.
- Invest in Prenatal Care – Prenatal care includes choosing a doctor to monitor your pregnancy and attending prenatal checkups. This can help you avoid a premature birth (babies born before 37 weeks of pregnancy). Premature babies tend to have more problems breastfeeding than full-term babies.
- Take a Breastfeeding Class – Many organizations and hospitals offer breastfeeding classes to teach you the basics. Our sister hospital, Texas Health Presbyterian Hospital Dallas, offers breastfeeding classes to help you prepare.
- Talk with Your Doctor – Discuss your wish to breastfeed with your doctor to ensure any previous injuries you have or any supplements, medications, or birth control you’re taking are safe for breastfeeding. Your doctor can also ensure that you’re able to breastfeed as soon as possible after delivery, which is important for your child’s first hour of life.
- Talk to Friends – Talk to your mom friends about breastfeeding or join a breastfeeding support group. They can offer support and provide guidance if you have any questions.
- Get Everything You Need – Purchase everything you’ll need to breastfeed, including nursing bras, nipple pads, nursing covers, nursing pillows, a breast pump, etc.
Pro Tip: Most health insurance companies will cover your first breast pump for free. You can find more information about this perk here.
Benefits of Breastfeeding for Your Baby
Your breast milk provides countless benefits for your baby’s health and development. It’s perfectly suited to provide the nutrients your baby needs as well as cells, hormones, and disease-fighting antibodies that can protect them from illness.
Your first milk, called colostrum, is considered “liquid gold” — not only for its rich, yellow color but because it’s packed full of nutrients and antibodies and helps newborns’ digestive systems grow and function properly. Over the first one to two weeks of your child’s life, your colostrum will change into mature milk containing the perfect combination of fat, sugar, water, and protein your baby needs to grow.
Preventing Illnesses
Your body will adapt the milk you produce over time. In fact, it’s believed that your baby’s saliva transfers a “status report” to your body to help it modify the nutrient and antibody content of your milk to meet your baby’s changing needs. Your body produces antibodies to fight the diseases present in your environment, making your milk custom-designed to fight the diseases your baby is exposed to as well.
According to the American Academy of Pediatrics (AAP), breastfeeding can reduce the chances of your baby developing the following illnesses and conditions:
- Asthma
- Bacteremia (the presence of bacteria in the blood)
- Diarrhea/vomiting
- Respiratory tract infections
- Necrotizing enterocolitis (a disease that affects the gastrointestinal tract in premature babies)
- Ear infections
- Urinary tract infections
- Late-onset sepsis in preterm infants
- Type 1 and type 2 diabetes
- Lymphoma, leukemia, and Hodgkin’s disease
- Childhood obesity
- Sudden infant death syndrome
Digestive Tract Development
Formulas can be hard on your child’s developing digestive tract because they are made from cow’s milk. It will take time for your baby’s stomach to adjust to digesting non-human milk. This is especially true for premature babies.
Breast milk, on the other hand, helps to line your newborn’s digestive tract with large amounts of bifidobacteria, or helpful bacteria that can prevent the growth of harmful organisms. Also, since breast milk comes directly from the breast, it is always sterile. This helps prevent digestive issues such as diarrhea.
Jaw Development
Breastfeeding promotes jaw development as it’s harder for your baby to get milk out of your breast than a bottle. The action of breastfeeding (sucking and stopping the flow of milk) strengthens your baby’s jaw and helps encourage the growth of straight, healthy teeth.
Physical Closeness
Physical, skin-to-skin contact during breastfeeding is important for newborns. Not only does it provide a sense of warmth, comfort, and security for your baby, but it boosts your body’s production of oxytocin, a hormone that helps keep you calm and aids the flow of breast milk.

Benefits of Breastfeeding for Mom
Breastfeeding also provides benefits for new moms. For starters, breastfeeding allows you to satisfy your baby’s hunger right away without having to worry about bottles, sterilizing bottle nipples, and mixing formula. It can also provide health benefits such as lowering your risk of developing type 2 diabetes, certain types of breast cancer, and ovarian cancer. Breastfeeding can also lead to decreased postpartum bleeding and help your uterus return to its pre-pregnancy state more quickly.
Breastfeeding may also help you lose weight after giving birth as your body draws calories stored during pregnancy to use in milk production. In the first three months of your child’s life, your body burns approximately 800 calories per day while breastfeeding, and burns even more calories in the following three months. This is especially helpful for women with gestational diabetes who are looking to return to a healthier postpartum body weight.
Aside from the physical benefits of breastfeeding, it can also save you money in the long run. Formula can cost more than $1,500 per year and gets more expensive as your baby grows and needs to eat more. But, as we mentioned, the nutrient content of your breast milk changes with your baby’s needs, and babies usually need the same amount of breast milk as they get older. Breastfed babies may also get sick less often, which can help keep health costs down.
Breast Milk Basics
Many first-time moms may have questions about how breast milk is produced, when it’ll first arrive, what will affect their supply, and how they should store any extra milk their baby doesn’t eat. Below we’ve covered some of the basic questions many moms have about breast milk.
How Breast Milk is Made
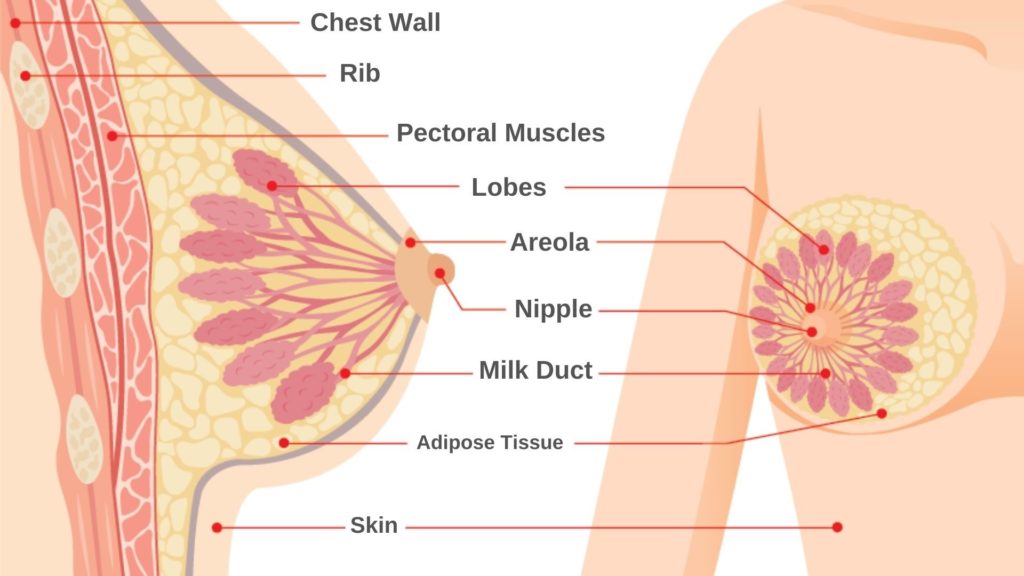
Knowing how your breasts actually produce milk can help you better understand how breastfeeding works.
Your breast is an organ that’s made up of several parts: alveoli cells, the areola (the dark area around the nipple), lobes, milk ducts, and the nipple. During pregnancy, you might notice that your breasts become fuller or more tender. This is a sign that the alveoli cells, which produce breast milk and are found within the lobes of your breasts, are getting ready to work.
The alveoli cells produce milk in response to two hormones: prolactin and oxytocin. Your prolactin and oxytocin levels go up when your baby suckles. This hormonal increase causes your breast to contract and move the milk through your milk ducts, which carry milk through the breast to the nipple/areola area.
The movement of milk through your breast triggers the “let-down reflex.” This reflex occurs when your baby begins to nurse and the nerves in your breast send signals to release milk into your milk ducts. The let-down reflex makes it easier to breastfeed and can happen anywhere from a few seconds to a few minutes after you begin breastfeeding. It can also occur several times while you’re breastfeeding.
Let-down can also be triggered when you hear your baby cry or when you’re simply thinking about your baby. Your body’s ability to trigger the let-down reflex can be negatively affected by factors such as anxiety, pain, embarrassment, stress, cold, excessive caffeine, smoking, alcohol, and some medications.
When Will Your Breast Milk Come In?
Your breast milk will arrive in three stages: colostrum, transitional milk, and mature milk. Your colostrum “liquid gold” is produced during pregnancy and is present when you first deliver. Colostrum contains a blend of protein, vitamins, and minerals that help defend against harmful bacteria and viruses. This early milk also stimulates your baby’s first bowel movement and reduces the risk of jaundice.
Your body likely won’t produce much colostrum, but don’t worry, your baby only needs a few teaspoons per feeding during the early days. Regularly breastfeeding from day one will help encourage your body to produce the next stage of milk within a few days.
The second stage of breast milk production is the transitional phase. Transitional milk will come in around three to four days after giving birth. It will resemble milk mixed with orange juice and contains lower levels of immunoglobulins and protein than colostrum. However, transitional milk contains more lactose, fat, and calories.
Around 10 days to two weeks after delivery, your body will begin to produce mature milk, which is thin, white, and sometimes slightly blue in color. Your mature milk is packed with all of the fat and other nutrients your baby needs to grow.

What Can Affect Your Breast Milk Supply?
There are two main factors that can affect how much breast milk your body produces:
- How completely milk is removed each time you breastfeed – Milk production increases when your breasts are empty. If your breasts store too much milk between feedings, milk production decreases.
- How often you breastfeed or pump to remove milk – Milk production increases with more frequent pumping or feeding.
Other factors that can cause low milk supply are waiting too long to start breastfeeding, supplementing breastfeeding with formula, an ineffective latch, taking certain medications, premature birth, maternal obesity, pregnancy-induced high blood pressure, and poorly controlled insulin-dependent diabetes. Previous breast surgeries can also affect your milk supply.
The main rule of thumb to ensure proper milk production is to feed often and to completely empty your breasts each time. If you find that your baby doesn’t empty your breasts after feedings, you can use the following methods to better empty them:
- Breast massage and compression
- Offering your baby both breasts when nursing
- Using a breast pump after nursing
A few things you can do to boost milk production include using a breast pump each time you miss a breastfeeding session, waiting to give your baby a pacifier until three or four weeks after birth, and limiting your consumption of alcohol and nicotine.
If you’re concerned about your milk supply, consult your doctor, a pediatrician, or a lactation consultant.
Storing Breast Milk
Using a breast pump to empty your breasts when you’re away from your baby or between feedings can help boost your milk production. However, this means you’ll need to properly store the breast milk you pump for future feedings.
It’s best to use breast milk storage bags, which are specifically made for freezing human milk. You can also use glass or BPA-free plastic bottles with tight-fitting lids. Do not use disposable bottle liners or other plastic liners to store breast milk.
The following are guidelines to follow when storing breast milk:
- After pumping, your milk can be kept at room temperature (up to 77° F) for up to four hours.
- Breast milk can be kept in the refrigerator for up to four days after pumping.
- If you’re unable to use the milk within four days, keep the milk in the freezer.
- When on the go, you can store breast milk in an insulated cooler for up to 24 hours.
You can find more resources on properly storing breast milk from WomensHealth.gov and the Centers for Disease Control and Prevention (CDC).

Breastfeeding Basics
Now that we’ve covered why it’s beneficial to breastfeed and how it works, it’s time to get into how to breastfeed your baby. Whether you’re a new mom or have had multiple pregnancies, you’re sure to find some tips and tricks for making breastfeeding less stressful and more rewarding for both you and your baby.
How Long Should Feedings Last?
While there is no set time for how long your feedings should last, many moms want guidance to know their baby needs to get enough milk.
Feeding sessions may last anywhere from 15 to 45 minutes, but your baby will ultimately let you know when he or she is finished. Your baby may take more or less time and need to feed longer in the early days or during growth spurts. The key is watching your baby for signals that they’ve had enough.
Watch your baby and stop feeding when he or she has let go of the nipple. If your baby doesn’t let go, end your feeding when the suck-swallow pattern slows down to around four sucks per one swallow. You’ll also know your baby has had enough when their hands are no longer fisted and they appear sleepy and relaxed. When your baby has finished with your first breast, burp them and move onto the other side. You can continue feeding until he or she stops feeding at the second breast.
You’ll ideally want to completely drain at least one breast during each feeding. This is more important than making sure your baby feeds from both breasts as the hindmilk — the last of the milk in your breast that your baby eats — is richer in both fat and calories. Wait until your baby seems done with the first breast and then offer, but don’t force, the second breast. If your baby drains one breast and doesn’t seem to want any more milk, you can start with the other breast next time you feed.
How Often Should You Breastfeed?
To start, you should breastfeed as soon as possible after giving birth as breastfeeding in these early hours is crucial for your baby. After delivery, you should breastfeed eight to 12 times in a 24-hour period, which translates to about every two to three hours. In the first few days after birth, you may need to feed every one to two hours. This ensures that your body produces enough milk and that your baby gets enough to eat.
It’s important to keep in mind that feeding patterns vary from baby to baby. If your baby is hungrier or more impatient, you may go an hour between feedings whereas a more easily satisfied baby might go three hours between feedings.
It’s best to feed your baby on demand rather than on a schedule. Watch for cues that your baby is hungry, such as increased alertness or activity, mouthing, rooting, and suckling. While crying is a sign of hunger, it’s often a late sign that your baby is hungry. This can make breastfeeding more difficult.
Your baby’s appetite might not pick up until around three days after birth. If there isn’t demand for feedings from your baby in the early days, you may have to initiate or push them to feed to make sure they get enough nutrients. For sleepy babies, your pediatrician may advise you to wake your baby every three hours for feedings.
Cluster Feeding
In the early days, your baby may want to “cluster feed,” meaning they feed several times close together and then go several hours without feeding. Your newborn may breastfeed every hour or several times in one hour, especially in the evening and at night. No matter the time of day, your baby should be satisfied after cluster feedings.
How Do You Know When Your Baby is Hungry?
As we mentioned, it’s best to feed on demand when your baby is hungry. A few signs your baby is hungry may include:
- Nuzzling against your breasts
- Sucking furiously on his or her hand, a shirt, or your arm
- Opening his or her mouth
- The rooting reflex
- Sucking on his or her lip or tongue
- Smacking his or her lips
- Short, low-pitched cries that rise and fall
The CDC further breaks down the signs that your baby might be hungry or full.

How to Know if Your Baby is Getting Enough
Your newborn’s tummy will be very small, especially in the first few days. In general, breastfed babies between 1-6 months old will eat 19 to 30 ounces of breast milk each day. This equates to 3 ounces per feeding if your baby feeds eight times per day. But keep in mind that each baby is different. At birth, your baby’s stomach can comfortably digest 1 to 2 teaspoons of milk. By day 10, their stomach will have grown to hold approximately 2 ounces of milk.
From birth to 3 months old, your baby will usually gain up to 1 ounce of weight each day. However, your baby may lose a small amount of weight in the first few days (up to 7-10% of their birth weight). From the second week on, gaining 4 to 7 ounces per week is typical. Your pediatrician will monitor your baby’s weight at their initial checkups.
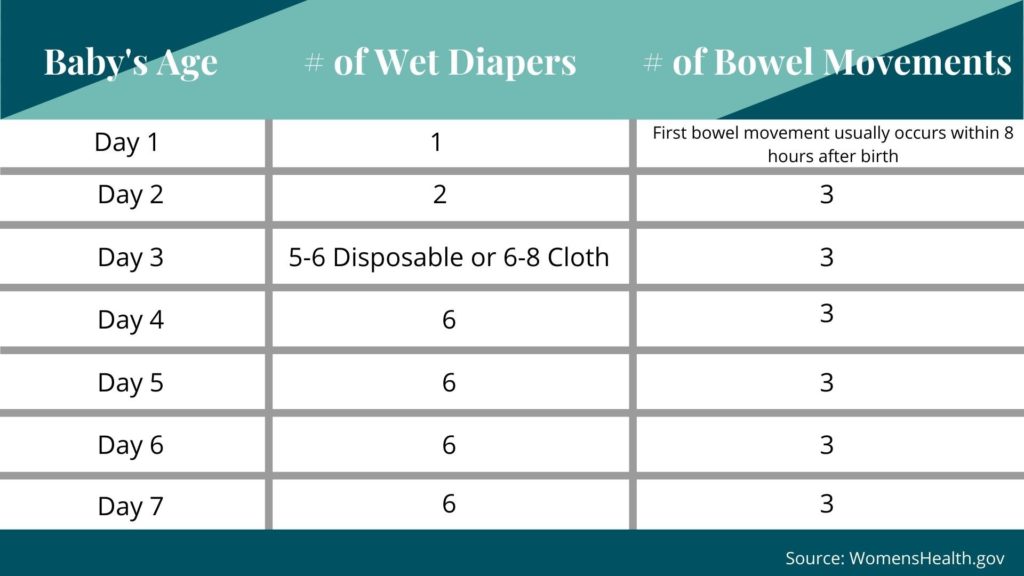
It can be challenging to know whether you’re producing enough milk and if your baby is getting enough to eat. However, there are a few indicators you can monitor — the first being your baby’s bowel movements.
You will know if your baby is getting enough milk if he or she has frequent bowel movements. Newborn stools are typically loose and change from black to brown to mustard-yellow in color in the first five days. By the third day after birth, your baby should have at least two to three bowel movements in a 24-hour period. By 5 days old your baby may have at least four yellow, seedy stools per day. Bowel movements will vary as your baby gets older, with some babies having one bowel movement per day and others having a bowel movement every few days.
Your baby’s dirty diaper can also serve as an indicator as to whether he or she is getting enough to eat. The following chart breaks down how many wet diapers you should expect each day if your baby is getting enough milk.
According to Sutter Health, other signs your baby is getting enough to eat include:
- Your baby’s urine is pale in color rather than deep yellow or orange.
- You can hear your baby swallowing the milk.
- Your baby is calm and relaxed after eating.
- Your breasts feel softer after feeding.
- Your baby switches between short sleeping periods and wakeful, alert periods.
How Long Should You Breastfeed?
The AAP recommends exclusively breastfeeding for the first six months of your baby’s life. At 6 months old, you can introduce solid foods in combination with breast milk. The AAP also recommends continuing to breastfeed beyond your baby’s first birthday and for as long as both you and your baby wish. Even though the benefits of breastfeeding as long as possible are widely proven, only 57.3% of women breastfeed their baby for the recommended six months with only 36.2% breastfeeding for one year.
The easiest way to wean your child off of breastfeeding is when your baby leads the process. But you should also make breastfeeding decisions that work for you and your lifestyle as well. Your decision to stop breastfeeding may be motivated by returning to work, your health, or simply feeling that the time is right. It’s ultimately up to you.
Are There Times When You Shouldn’t Breastfeed?
If you take regular medications or are sick, it’s best to check with your doctor before breastfeeding. Medications that are safe to take during pregnancy are typically safe to take while breastfeeding, but it’s always best to check. You should also consult your doctor if your baby shows any signs of a reaction to your breast milk, such as diarrhea, excessive crying, or sleepiness.
It’s OK to be worried about breastfeeding when you’re under the weather; however, you can usually breastfeed when you’re sick or when your baby is sick. If you need extra rest, it’s always okay to pump or hand express breast milk for someone else to feed the baby via a bottle.
If you have the flu, it’s important that you do not touch or be near your baby so that you do not infect him or her.
Latching Tips
Ensuring a good latch is important for successful breastfeeding. When your baby is properly latched onto your nipple, it’s easier for them to get the milk they need and ensures comfort for both you and your baby.
One method of latching involves allowing your baby to begin the process of searching for your breast to feed. Called baby-led breastfeeding, this style of breastfeeding gives your baby the chance to lead and follow his or her natural instinct to suck.
A few ways to help your baby relax and naturally form a latch include:
- Creating a calming environment by reclining on pillows or relaxing in another comfortable area
- Relaxing and holding your baby skin-to-skin between your breasts before breastfeeding
- Letting your baby lead when he or she is hungry. Your baby may bob his or her head against you, try to make eye contact, or squirm around.
- Supporting your baby’s head and shoulders as he or she searches for your breast
- Allowing your breast to hang naturally so that your baby’s chin rests on your breast, allowing them to get a full mouthful
If the baby-led method does not lead to a successful latch, trying tickling your baby’s lips with your nipple to encourage him or her to open their mouth, pulling your baby close so that their chin and lower jaw moves into your breast, or aiming your baby’s lower lip as far from the base of the nipple as possible so that they take a large mouthful of breast.
WomensHealth.gov details signs that you have achieved a good latch as well as positions to help you get comfortable and support your baby while breastfeeding. The Bump also provides illustrated demonstrations of different successful breastfeeding positions.

Getting Help
According to a survey conducted by the UC Davis Medical Center, 92% of new mothers experienced problems while attempting to breastfeed their baby in the first three days after giving birth.
This goes to say that experiencing issues while breastfeeding is common. Whether you’re struggling to get your baby to latch, having issues with milk production, or are experiencing issues such as mastitis or breast engorgement, there are plenty of resources you can use to get the help you need.
Lactation Consultants
International Board-Certified Lactation Consultants (IBCLCs) are certified breastfeeding professionals with the highest level of knowledge and skill in providing breastfeeding support. IBCLCs can help with a wide range of breastfeeding issues that you may experience after giving birth, such as nipple and breast pain, inadequate weight gain, longer than normal feeding sessions, and more.
Our sister hospital, Texas Health Presbyterian Hospital Dallas, has lactation consultants on staff to help you breastfeed your baby after delivery. You can also find a lactation consultant in your community through the International Lactation Consultant Association.
Other Resources
Consult your baby’s pediatrician about any breastfeeding issues you may have. You can also ask your doctor to recommend a breastfeeding peer counselor, a woman who has breastfed her own baby and can help other moms with breastfeeding. Many states offer Women, Infants, and Children (WIC) programs that offer peer counseling support as well as supplies for low-income families.
Doulas, professionals who provide guidance both during pregnancy and postpartum, are also trained in breastfeeding and can help you learn how to best feed your baby.
La Leche League International is an organization dedicated to helping breastfeeding mothers around the world by providing support, education, and information. Breastfeeding USA and the Nursing Mothers Advisory Council both provide educational resources for mothers as well as local breastfeeding centers and support groups. The National Women’s Health and Breastfeeding Helpline (1-800-994-9662) has trained women’s health specialists and breastfeeding peer counselors available Monday through Friday, 9 a.m. to 6 p.m. ET, to answer any questions you may have.
Other breastfeeding mothers are a great resource for support, reassurance, and breastfeeding tips. You can also try searching for blogs, message boards, chats, or social media groups dedicated to new mothers looking for resources and medical advice.
If you’ve sought help and are still having problems breastfeeding your baby, know that breastfeeding isn’t an all-or-nothing endeavor. Your doctor may recommend supplementing breastfeeding with formula or switching to full-time formula-feeding if necessary.
Using Formula
While doctors agree that breast milk provides the most nutritional value for your baby, mothers may choose to formula-feed their baby out of comfort, because their lifestyle necessitates it, or due to a special medical situation.
For moms who can’t breastfeed, formula is a healthy alternative that can provide your baby with the nutrients they need to grow and stay healthy. It’s important to only use commercially prepared formulas as they are produced to mimic the complex combination of proteins, sugars, fats, and vitamins found in breast milk.
Benefits that formula-feeding your baby can provide include:
- Convenience – Either parent or another caregiver can feed your baby a bottle at any time (although this is also true for women who pump their breast milk).
- Frequency of Feedings – Formula is less digestible than breast milk, which means formula-fed babies usually need to eat less often than breastfed babies.
- Diet – You don’t need to worry about what you eat or drink when using formula.
On the flip side, there are some common challenges mothers may face while formula-feeding.
- Lack of Antibodies – Formulas do not transfer antibodies to your baby like breast milk does. This takes away the added protection against infection and illness.
- Required Planning – Formula-feeding requires that you buy formula, prepare it, and have the necessary supplies on hand (bottles and nipples) when your baby is hungry. Unlike breastfeeding, which can occur at any time, it takes time and organization to prepare formula for your baby.
- Cost – As we mentioned before, formula can be expensive, costing around $1,500 in your baby’s first year of life. Powdered formulas are often the most affordable, while concentrated, ready-to-feed formulas are more costly. Specialty formulas for babies with certain allergies or intolerances can be the most expensive.
- Gastrointestinal Issues – Formula may make your baby gassier or cause firmer stools that can lead to constipation.
If you make the choice to formula-feed, the CDC provides guidance on properly preparing and storing your formula.
What to Eat While Breastfeeding
It’s normal to wonder if what you eat and drink while breastfeeding can affect your breast milk and consequently your baby. Luckily, for most women, there are only a few foods that you should limit while breastfeeding due to negative effects they could have on your baby — everything else is fair game. Even better, many foods can actually boost your milk production!
We’ll walk you through which foods you might want to consider adding to your diet as well as those you might want to limit until after your baby stops breastfeeding.
Foods That Can Increase Milk Production
Some foods, called lactogenic foods, can increase the nutrient content of your breast milk as well as the supply of breast milk your body produces. As with any part of your diet, you don’t want to overdo it on the lactogenic foods. Overproduction of breast milk can lead to issues such as breast engorgement, clogged milk ducts, or mastitis. But incorporating some of these common foods into your diet could lead to positive outcomes for both you and your baby.
You can find a list of lactogenic foods in the below graphic. For more details on the benefits these foods provide, check out these resources:
- How to Increase Breast Milk: 7 Foods to Eat
- Foods to Increase Breast Milk Supply
- 5 Foods That Might Help Boost Your Breast Milk Supply
- How to Eat a Healthy Breastfeeding Diet
For a fun, and delicious, way to increase milk production, try making lactation cookies likes these from Food.com!

Foods to Limit While Breastfeeding
There are very few foods you need to eliminate from your diet while breastfeeding. However, there are a few things you should limit, such as alcohol and caffeine, that can impact your baby’s health and your milk supply when consumed in large quantities.
- Alcohol – Having two alcoholic drinks per week is generally considered safe while breastfeeding. While alcohol can be passed to breast milk, it’s usually in very small amounts. In general, once you no longer feel the effects of consuming alcohol, it’s safe to feed.
- Caffeine – Too much caffeine can overstimulate your baby and cause irritability. Three or fewer caffeinated beverages per day is considered safe. Like alcohol, caffeine can pass through your beat milk so it’s best to consume caffeine after a nursing session is finished.
- Fish – Fish known to have high levels of mercury, such as shark, swordfish, tilefish, and king mackerel, should be avoided while breastfeeding. Other fish varieties usually contain small enough amounts of mercury that the benefits of eating them outweigh any risks. Eating 12 ounces of low-mercury fish per week (such as shrimp, salmon, pollock, or catfish) is considered safe.
- Chocolate – Too much chocolate can overstimulate your baby and cause irritability.
- Herbs – Peppermint, parsley, and sage typically get a bad reputation when it comes to breastfeeding as some women believe they can decrease milk production. However, you’d have to consume very large quantities of these three herbs for them to affect you or your baby. Using them to season or flavor foods is perfectly safe.
Certain foods such as soy, dairy products made from cow’s milk, gluten, eggs, peanuts/tree nuts, and citrus may need to be removed from your diet if you notice your baby is negatively affected by them. These foods are the culprits behind many common food intolerances. If you notice a negative reaction from your baby (such as gastrointestinal issues or irritability) after consuming one of these foods, simply removing it from your diet should resolve the problem.

Which Medications Are Safe to Take While Breastfeeding?
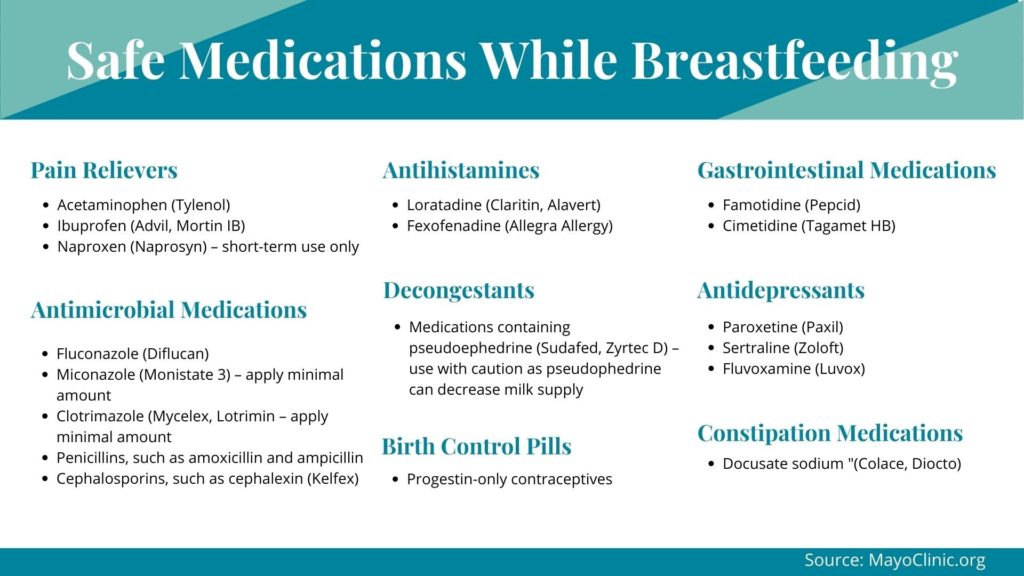
Almost any medication that is present in your blood can transfer into your breast milk. Most medications, though, become concentrated in breast milk at low levels that pose no risk to your baby. However, it’s always best to review with your doctor medications you’re taking, associated risks and considerations before you begin breastfeeding.
While the benefit of continuing to take medications while breastfeeding, especially for chronic conditions, outweighs any potential risks, there are some medications that aren’t safe while breastfeeding. In these circumstances, your doctor may recommend alternative medications or breastfeeding when the medication is present in your breast milk at low levels.
In some cases, your doctor may recommend that you stop breastfeeding temporarily or permanently while taking certain medications. If you have advance notice, you can pump in addition to feedings and store milk to use while you’re unable to breastfeed.
Medications That Are Safe
According to the Mayo Clinic, the following medications are considered safe to take while breastfeeding. (This is not a complete list of all safe medications.)
Medications to Avoid
Some medications that your doctor may advise you to stop taking while breastfeeding include:
- Bromocriptine (Parlodel) – a drug used to treat Parkinson’s disease
- Chemotherapy drugs
- Ergotamine – used to treat migraine headaches
- Lithium – used to treat manic-depressive illnesses
- Methotrexate – used to treat arthritis
- Abused substances such as cocaine, PCP, amphetamines, heroin, and marijuana
- Nicotine
Great Resources for Breastfeeding Moms
- American Academy of Family Physicians
- American Academy of Pediatrics
- American College of Obstetricians and Gynecologists
- Human Milk Banking Association of North America
- International Lactation Consultant Association (ILCA)
- La Leche League International
- National Center for Education in Maternal and Child Health
- Wellstart International
- World Alliance for Breastfeeding Action
- World Breastfeeding Week
- The Bump
- What To Expect
Above All Else, Consult Your Doctor
If you have any questions about breastfeeding, consult your Walnut Hill OBGYN or your baby’s pediatrician. They can provide assistance, education, and resources as well as help guide you throughout your pregnancy. Feel free to contact us with any questions or concerns you may have.

